| |
 |
Archive for Diabetes
February 14, 2010 at 9:22 am
· Filed under Diabetes, General Nutrition & Wellness, Professional Interest
Happy Valentine’s Day! I wanted to take this day to discuss a subject that is near and dear to my heart. I am a Registered Dietitian and, yes, nutrition is a love of mine. However, I would have to say that my true passion lies in helping those who have diabetes live healthier and happier lives.
Chances are that you have a family member, friend or at least know of someone who has the diabetes. In the past 25 years, the rate of diabetes in the United States has more than tripled. Currently, 21 million, or seven percent of the U.S. population has this chronic disease (Source: NIDDK).
People who happen to have diabetes should not be called “diabetic”. In contrast, they should be referred to as “having diabetes”. It really makes me cringe when I hear an individual being identified as “the diabetic”. I hear it in both the lay as well as health care settings. It is especially displeasing when I hear it used in the medical community. Coming from a professional perspective, this is awful. People with diabetes are people. They are people who just happen to have diabetes.
It’s not about being politically correct. It’s about semantics. We need to consider the person. They are much more than their disease. As the wife of someone who has diabetes, it makes me even more upset. John is not a “diabetic”. John is a person — a wonderful person who lives a healthy, full life and has many different interests and hobbies. He just happens to have diabetes. John says it does not bother him to be called “diabetic”. “That’s what I am”, he will say. But, he does think it’s peculiar and amusing to call an object “diabetic” such as “diabetic yogurt”, “diabetic socks” or “diabetic shoes”. “The shoes don’t have diabetes”, he will say jokingly.
The term “diabetic diet” is even no longer used. The American Diabetes Association (ADA) eliminated the use of the terms “Diabetic Diet” and “ADA Diet” over ten years ago. They stated that there is no one diet for people with diabetes and that meal plans need to be individualized.
In that same sense, people with diabetes are individuals — individuals who happen to have diabetes. Please call them by their names and not a disease.
It’s Your Health. It’s Your Life. Make that change!
~ Angie
Permalink
January 5, 2010 at 6:15 am
· Filed under , Diabetes
We checked Jonathan’s blood sugar last night. He had asked us to. He prefers us to do this while he is asleep. There is no struggle and he does not ever remember it. It is something that John and I have been doing about every 6 months or so with him. Of our two children, he is the child that we worry the most about getting Type 1 Diabetes. The thin body frame. The mood swings when he goes more than 4 hours without eating. Lately it has been extreme exhaustion every night around 6 or 7 pm and a voracious appetite that has had us concerned.
Jonathan will be nine next week. He asks a lot about diabetes. He is always very concerned about John and what his blood sugars are doing. “What’s your blood sugar, Daddy?” he will ask each time he hears the click of the lancing device coming from the kitchen. He has stopped asking “Is that good?” when John tells him the readings as he now knows where John’s levels should be.
John and I had conversations before we decided to have children. We knew that our children would run the risk of developing diabetes. So, we checked the stats… an 8% chance if the father has Type 1 Diabetes and a 6% chance if the mother has Type 1 Diabetes. 8% is not bad. A 92% chance that they will not have diabetes sounds even better, we thought. Besides, if our children ever did ever develop Type 1, who better to have as parents than two Certified Diabetes Educators who have actually lived with diabetes for quite some time. And, although it is a chronic disease that will not ever go away, it is a disease that is controllable.
Still, in the back of our minds, the concern is always there. We hope that they never will develop diabetes. John has said that he would have an extremely difficult time, emotionally, if this were to ever happen.
Jonathan knows that we want to check his blood sugar when he starts the get thirsty, tired or has been acting up. So last night when he was falling asleep before dinner at 6 pm, he asked us to check his blood sugar while he was asleep that night.
So we did. 120 two hours and a half hours postprandial. That’s ok but I’d be more comfortable with a number lower than that. A fasting level over 126 or a random (any time of the day) level over 200 is the diagnostic criteria for diabetes. We will schedule his annual physical and stay on top of this.
~Angie
Permalink
November 12, 2009 at 6:43 am
· Filed under , Diabetes, General Nutrition & Wellness, Nutrition
November is National Diabetes Awareness Month. This is an opportunity to recognize this widespread disease that can result in serious and debilitating complications, such as heart disease, stroke, kidney disease, blindness, and amputation. In the United States, 24 million people or 7% of the population have diabetes. Another 57 million Americans, or 29% of the population, have pre-diabetes. The incidence of diabetes in North Carolina is especially high as North Carolina ranks tenth in the nation.
Diabetes is an expensive disease. One out of every five U.S. health care dollars is spent caring for individuals with diabetes. The total annual economic cost of diabetes in 2007 was estimated to be $174 billion. In fact, over the past five years, the cost has risen more than $8 billion each year.
The prevalence of diabetes in the U.S. is also rising. It has more than tripled over the past 25 years. The CDC estimates that every 21 seconds, someone in the US is diagnosed with diabetes. If things continue at this rate, 1 in 3 children born today will develop diabetes within their lifetime. Research has shown that obesity is the main reason for this increase.
Besides obesity, additional risk factors for diabetes include:
- Sedentary lifestyle
- Unhealthy eating habits
- Age over 45 years
- Family history of diabetes
- African American, Latina, Native American, Asian American, Pacific Island ethnicity
- Women who have delivered babies nine pounds or more at birth.
The good news in all this is that diabetes is a controllable disease. We can’t control our genetics, ethnicity or age, but we can control unhealthy eating habits and a sedentary lifestyle. Complications are decreased when blood sugar control is managed through health eating and physical activity. Research has shown that for every 1% reduction in Hemoglobin A1C (A1c), the risk of developing eye, kidney, and nerve disease is reduced by 40%. The A1c is an estimate of average blood sugar over the previous three months. What this means is that if your average blood sugar is lowered by just 30 points, your chance of any potential complications is almost cut in half.
If you have diabetes, pre-diabetes or are even at high risk of developing diabetes, find a Registered Dietitian, preferably one who is a Certified Diabetes Educators (CDE). A CDE is a health care professional that teaches people with diabetes to manage their condition. Formal education, years of practical experience, and a Board Examination are required prior to becoming a CDE. RD/CDE’s will help you to learn the tools, skills and emotional support necessary to control blood sugar and decrease the risk of long term complications.
It’s Your Health. It’s Your Life. Make That change!
~ Angie
Permalink
April 22, 2009 at 4:51 am
· Filed under Diabetes, Professional Interest
I was lucky enough to be invited to attend the Johnson & Johnson Diabetes Institute in Milpitas, California at the beginning of April. The Institute is a 2 day intensive diabetes education/training session to help Diabetes Educators, Nurse Practitioners, Physician Assistants, & other Health care providers find innovative answers to to some of the challenges facing diabetes care. Topics ranged from Insulin Pump Therapy to Continuous Glucose Management to Reimbursement issues to Behavioral Change Techniques. Overall, the session was very enlightening for me. I was able to meet with Diabetes Educators from around the United States and share ideas on improving diabetes care.
One session I really enjoyed involved the topic of diabetes medications. With Type 2 Diabetes, the patient is usually diagnosed some time after diabetes has developed. Treatment is normally started with oral medications (pills) along with lifestyle & diet change. Insulin is usually a last-ditch effort to improve blood sugar control. However, Type 2 Diabetes is a progressive disease. When Type 2 is diagnosed, many years may have passed since the patient truly developed the disease. In that time, the pancreas may have already maxed out its insulin production. What that means is that insulin may be needed sooner than would be expected. What that also means is that insulin starts should not be seen as patient “failures”. The nature of Type 2 Diabetes progression will eventually lead to that, regardless of overall control. Therefore, it is important to at least start talking about insulin use soon after the diagnosis is made. There is no question that initiating insulin brings up many fears in patients and providers alike. But if you look at the types of insulin that are available today, we have significantly more choices and options than we did just 10 or 15 years ago.
Insulin is a medication that could be considered much more natural than its oral counterparts. Insulin is simply a hormone made by the pancreas to help the body utilize energy. With insulin, you may run a higher risk of having hypoglycemic (low blood sugar) episodes but those can be minimized. In fact, some oral agents are contraindicated in geriatric patients or those with kidney, liver or heart disease. There is less risk to the liver and kidneys with insulin as it is not excreted through these organs like many of the oral agents. A major benefit to using insulin is that it allows you to tailor your approach to blood sugar control. It gives you the opportunity to fine tune adjustments and get exactly what you need, when you need it. Of course, when using insulin you must still balance between exercise and proper food intake to get the maximum benefit!
We need to make sure that we don’t view the use of insulin as a failure. Insulin should be used more freely as a means to achieving better blood glucose control earlier on in the treatment of diabetes. Once on insulin, we would encourage more frequent blood glucose testing. This gives the patient instant feedback on how his or her therapy is progressing. We have multiple tools available to us. We must use them more efficiently.
If you are not meeeting your diabetes health related goals, talk to your physician about the possible use of insulin. There are risks and benefits associated with any medication change, but if it enables you to control diabetes better, the benefits will far outweigh the risks. Take control of your diabetes!
It’s Your Health! It’s Yor Life! Make That Change!
Johnикони
Permalink
March 24, 2009 at 8:20 am
· Filed under , Diabetes, Professional Interest

Today, Tuesday, March 24th is American Diabetes Alert Day. The American Diabetes Association has indicated this day as a “wake up call” to the seriousness of this disease.
24 million adults and children in our country have diabetes. About 25% of these do not even know that they have it. However, early diagnosis is critical to treatment as uncontrolled blood sugars can lead to:
- Heart Disease
- Blindness
- Kidney Failure
- Stroke
- Lower limb amputations
- Death
Diabetes prevalence in the U.S. has more than tripled over the past 25 years. Research has shown that obesity is the main reason for this increase. Besides obesity, additional risk factors for diabetes include:
- Sedentary lifestyle
- Unhealthy eating habits
- Age over 45 years
- Family history of diabetes
- African American, Latino, American Indian, Asian American or Pacific Island ethnicity
- Women who have delivered babies weighing 9 pounds or more at birth.
Could you be at risk? Take the free Diabetes Risk Test at www.diabetes.org/alert or call 1.800.342.2383. If you have diabetes or are at high risk of developing diabetes, working with your physician and a Certified Diabetes Educator will help you to be better able to control your blood sugars. Doing so will prevent the complications that can occur when blood sugars are uncontrolled.
Nutrition Pair, LLC is a married couple of Registered Dietitians and Certified Diabetes Educators who, along with the care of your physician, can help those who have diabetes, prediabetes or who are at high risk for developing diabetes. We know diabetes on both a professional and personal level as John has had Type 1 Diabetes for the past 18 years. Contact us at http://www.nutritionpair.com/index.php?link=contact .
It’s Your Health. It’s Your Life. Make That Change!
~ Angie
Permalink
November 11, 2008 at 6:08 am
· Filed under Diabetes
Are Sugar-Free Products Better?
When taking a trip to the grocery store, you will find many products that are labeled “sugar free”. But, take caution as these products are not always an ideal choice when you have diabetes. “Sugar free” products can actually be quite deceiving. A common error that we have observed as diabetes educators is that many people read labels for the amount of sugar instead of for the amount of total carbohydrate. Even if there are zero grams of sugar in a product, the food can still have an impact on your blood sugar level. The reason for this is that it is that total carbohydrate, not only sugar, affects blood sugar levels.
Carbohydrates (Carbs) can be classified as either simple carbs or complex carbs. Simple Carbohydrates generally include foods with added sugars like regular sodas and sweets. They are called “simple” because the body does not have to perform much in the way of digestion to break them down. Simple carbs offer very little nutritional value. Complex Carbohydrates include foods that occur naturally and without processing. Foods such as fruits, starchy vegetables, whole grain breads and rice would fall into the complex category. While complex carbs will raise blood sugar levels just like simple carbs, they differ in that they contain more vitamins, minerals and fiber than simple carbs. Because of that, complex carbs are a better choice than simple carbs.
You will find sugar (simple carb) listed on the Nutrition Facts label. However, the only complex carb that you will find listed is fiber. Thus, a product may not have sugar but it can still have other carbohydrates. It is important to look at the total carbohydrate content, not only the sugar content, when you are reading a food label.
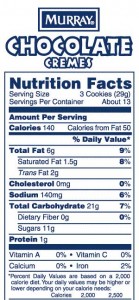
As an example, take a look at these two labels. This is a comparison of a Sugar Free and a Regular Version of cookies:
 Sugar Free Cookie Food Label 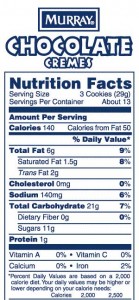 Murrays Regular Chocolate Creme Cookies Note the difference between the two cookies: other than the nutrition label showing that the sugar-free cookie contains 0g sugar, there is very little difference. Knowing that you need to look for total carbohydrate instead of sugar makes all the difference. The total carb in the sugar free cookie is 19 grams while the total carb in the regular cookie is 21 grams. (Two grams of carb will not make a notable difference in your blood sugar level.) One carb serving/exchange is equivalent to 15 grams of carbohydrate. Although carbohydrate needs are very individualized, most people with diabetes will need to keep their mealtime carbs between 30 to 60 grams (2 to 4 servings/exchanges) and their snacks between 15 to 30 grams (1 to 2 servings/exchanges). Registered Dietitians who are Certified Diabetes Educators, such as John and I at nutritionpair.com, can assist you in determining your individual carbohydrate needs.
Back to the cookies—I should note the price per cookie. The sugar-free cookies cost 15 cents per cookie and the regular cookies cost 4 cents per cookie. The sugar-free cookies cost almost four times as much as the regular cookie! As you can see from the comparison above, there is very little difference in the impact the two different products would have on your blood sugar level. Your blood sugar reading would likely be the same after the sugar-free cookies as it would after the regular cookies. As you can see, you really don’t need to spend the extra money on “diabetic” or “sugar-free” products when you have diabetes. Just be a label reader and look at the total carbohydrate instead of the sugar. While you’re at it, check to make sure the product is low in saturated fat, high in fiber and high in vitamins and minerals. But, remember, the healthiest foods do not even have a nutrition label on them (hint: they are in the produce section!!!).
~ Angie
Permalink
July 23, 2008 at 5:36 am
· Filed under Diabetes
I was sitting around thinking the other day about the Tom Hanks movie, “Cast Away”. How do you think that movie would have changed had the main character had Type 1 Diabetes? I’m pretty sure he would not have lasted 4 years on a remote island. He may not have lasted 4 weeks. I think back to right before I was diagnosed. The extreme fatigue, cramping, constant urination, and rapid weight loss. I can remember just how bad I felt. That is something I would not want to experience again. But how would I survive if I became stranded on some remote island, or if I became lost in the woods or mountains while hiking? When I travel, I always carry my Diabetes supplies in a large zip-lock bag stored in my backpack. That way if I end up on an airplane that goes down in the ocean, I know that I will have safe supplies. While I always carry extra insulin, syringes, & test strips when I travel it is usually only a couple of extra days worth of supplies. Not enough to last me months! Imagine how you would find food, test your blood sugar, keep medication from getting too hot or too cold. Honing your Diabetes Survival instincts are just as important to us as it was for Tom Hanks’ character to talk to the volleyball!
Having Type 1 diabetes means we must be on guard everyday. We must plan for an emergency while living in the moment. It’s like living on a constant episode of “Survivor”. There are no breaks from Diabetes. If we can stay on top of our diabetes, then we should be able to stay on top of the other stuff that happens in life. Forget the potential complications associated with having diabetes. Living well day to day requires us to be at the top of our game. When you get right down to it, Diabetes is a life & death proposition. But isn’t life anyway?
To everyone with Diabetes: Keep surviving. Keep thriving. Keep living life and keep enjoying each & every day you have. Having Diabetes might be scary, or be an inconvenience but there are some bigger problems in life. Update & review your Diabetes Survival plans & supplies. Make sure others are aware of your medical needs. Then ask yourself, “How would I survive with Type 1 Diabetes if stranded alone?”
It’s Your Health. It’s Your Life. Make that Change!
~John
Permalink
December 17, 2007 at 11:12 am
· Filed under Diabetes
John and I recently became Certified Pump Trainers for the OmniPod insulin pump. The OmniPod is the Insulet Corporation’s Insulin Management System. It is the first and only wireless insulin pump. The OmniPod consists of a “pod” that attaches to the skin and delivers insulin via communication with a personal data manager (PDM).
Some of the things we really like about the pump are:
• There are no wires or tubes
• The PDM has a built-in blood glucose monitor (less items to carry with you)
• No needles are ever seen by the wearer as the pods have an automated cannula
insertion system
• No need to detach for swimming, showering, etc
• The only supplies needed are the pods and the insulin. With other insulin pumps
you must order tubing, insulin, needles and needle insertion systems.
The OmniPod is a relatively new insulin delivery device. It received FDA approval in 2005. Last year, the company won three awards for the device: a Gold Medical Device Excellence Award from Canon Communications LLC, a New England Innovation Award from the Smaller Business Association of New England, and a Gold Industrial Design Excellence Award from the Industrial Designers Society of America.
It is a really cool design and John and I are excited to start training new OmniPod clients! For more information on the OmniPod, go to http://www.myomnipod.com/.
It’s Your Health. It’s Your Life. Make That Change!
~ Angie
Permalink
November 16, 2007 at 9:12 am
· Filed under Diabetes
John and I took part in another radio show on November 2nd with host Frank Roberts on Radio Cafe Hertford 103. Diabetes was our topic of discussion as November is Diabetes Awareness Month.
Some of the important points that were made include:
-14.6 million Americans have diagnosed diabetes
-6.2 million Americans have undiagnosed diabetes
-54 million Americans have Pre-diabetes
This means that approximately 7% of our population has diabetes and 15% have pre-diabetes. In other words, almost one in four Americans have either diabetes or pre-diabetes!
You can listen to all of our previous radio shows through this link:
http://www.rch103.com/?s=lamberson
It’s Your Health. It’s Your Life. Make That Change!
~ Angie
Permalink
October 31, 2007 at 4:29 pm
· Filed under Diabetes
It happened again today. This makes the third time this week. However, it is always worse when it happens first thing in the morning. Whenever John sleeps later than I have, I know that something is wrong. We usually go about day to day without any problems with John’s diabetes. But, every once in a while we get a reminder of how serious diabetes can be.
John is always active, but he has been especially more so lately. He is running much these days and gearing up for basketball season.
I thought maybe he was just tired, so I let him sleep. Even after I got out of the shower he was still asleep. I then heard our six year old calling me from his room. “Mommy, why isn’t Daddy up yet?”, he asked (Jonathan is always up at 6 am and will keep John company during his morning work outs). Jonathan went into our bedroom and I could hear him talking to John. He came out to the kitchen and said, “Mommy, I need the thermometer, Daddy is not acting right”. I knew right then that it was his blood sugar. I felt guilty for not having tried to wake him up earlier. I walked into the bedroom and John looked at me with a glazed look and said “Wheww! Wheww!”. He sounded like a college boy who had just come in from drinking all night. I went to go get juice. Yes, you should check your blood glucose first to see what it is before you treat it. However, when John is hypoglycemic, this is almost impossible to do as he will often refuse. Because I did not get a response from him, I knew it was truly low. Right around this time our four year old daughter woke up ready to eat (as usual!). Jonathan took over and gave John a juice box. All the while, John is still in bed yelling, “Whew! Whew!”. Jonathan is quite confused but thinks it is funny. “Daddy says he doesn’t know who I am, I keep asking him and he won’t answer me”. I used this as a teaching moment for Jonathan and told him what to do if this happens when I am not around: “If he does not answer you, call 911. If he can still talk to you, give him some juice. If he won’t drink it, call 911.”
Diabetes makes me so angry sometimes. You cannot reason with John when his BG is low. I’m lucky if I can get him to drink juice, forget about getting him to eat something or take glucose tabs (by the way-4 glucose tabs is the best treatment for hypoglycemia). He will often spit out or spill what I give him. This makes me even more scared and angry because I know that if we don’t get any carb in his body that he will lose consciousness. I have even in the past had to forcibly squeeze glucose gel into his mouth. But it is nearly impossible to hold down someone who is 50 pounds heavier than you are and is fighting you because he does not understand what you are trying to do to him. We do keep Glucagon in the house (and this I recommend for all people with diabetes). However, the only way I could use this would be if he were totally passed out as I can’t imagine trying to give him an injection if he were fighting me. Fortunately, we have never had to use the Glucagon but we do keep it in the house and take it with us whenever we travel.
John eventually came around, got up and was able to make his own breakfast and get to work. I knew he did not feel well, though he would not admit to it. He always talks about how hypoglycemia is a horrible start to your day-similar to a hangover. He will usually have a headache all day.
The best thing for us to do is to try to prevent this from happening again. Hypoglycemia is one of the biggest risks of tight blood glucose control. Checking blood sugar prior to bedtime and having a bedtime snack of at least 1 protein and 1 carb if your blood sugar is under 100mg/dl before you go to bed is always a good idea if you have had an especially active day.
~Angie
Permalink
« Previous Page — � Previous entries « Previous Page · Next Page » Next entries � — Next Page »
|
 |
|
|